|
TMC Pulse magazine did a wonderful feature on a boy and his family, telling their story leading up to his endoscopic hemispherotomy as well as life after the surgery.
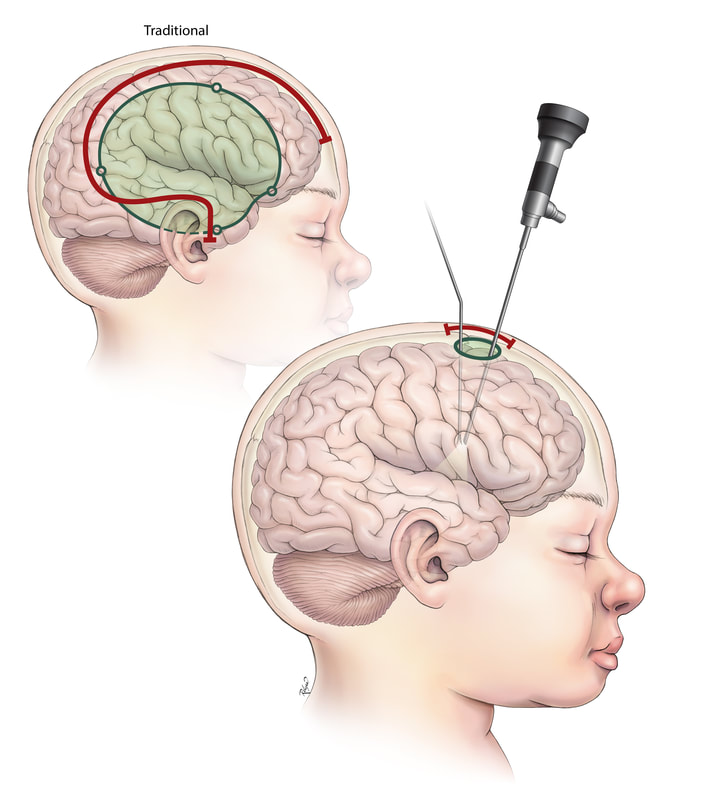
We have a new epilepsy surgery offering to our patients: endoscopic hemispherectomy. I am excited to see how remarkably well patients recover after endoscopic surgery! Unlike traditional open hemispherectomy/hemispherotomy surgery which involves a large craniotomy (skull bone opening) and a large question-mark-shaped incision on the top and side of the head to disconnect the left hemisphere from the right hemisphere, I can perform the hemispherectomy surgery through a small opening and with the help of an endoscope – a camera used in the procedure. The scar involves only a small opening at the top of the head. This smaller access surgery translates to less blood loss, less pain/discomfort, and quicker recovery. This type of surgery is relatively novel, as it has been reported by only two other centers in the world - one in India and one in Detroit. This type of minimal access surgery to treat seizures fits with our program's expertise with minimally invasive surgery and enhanced recovery, and expands the comprehensive offering of our multidisciplinary comprehensive pediatric epilepsy surgery program. We focus on delivering individualized care -- offering the right diagnostic workup, the right treatment, the right surgical plan tailored for each patient. This new endoscopic surgery application was possible with intricate understanding of anatomy with my experience with open hemispherectomy surgeries, which I have written about in textbooks. Recently, I have spent time developing and perfecting these minimal-access surgical approaches in the anatomy lab, anticipating and working out all contingencies before offering this novel endoscopic surgery to patients. While the epilepsy surgery program in my group has been known for laser ablation surgeries and traditional open surgeries, we continue to learn from our collective experience. We recognize that not every disease process or surgical goal can be addressed with the laser. There was room for development of better surgical techniques – something in between a laser and a traditional open surgery. Incorporating the use of a camera – the endoscope – gave a way to see what I need to see, while allowing for a smaller opening to safely achieve what needed to be done in surgery. Epilepsy surgeries I offer through an endoscope include corpus callosotomy and hemispherectomy. Illustration developed with our talented medical illustrator, Kathy Relyea.
I returned from my 6th annual trip as visiting pediatric neurosurgeon to Kijabe Hospital in Kenya this November.
My mentor Dr. Leland Albright and his wife Susan Ferson (the best nurse practicitioner ever) spent many years developing pediatric neurosurgery in Kijabe. Read their amazing blog here. While every year I am grateful for the privilege of serving in a place that has such need, there were many things that made this visit special: I spent time with Dr. Albright, who was returning to visit Kijabe for the first time after more than 2 years away. Dr. Kathryn Wagner, a neurosurgery resident from Baylor College of Medicine, came to Kijabe with us. In 2 weeks, Kathryn took care of a variety of neurosurgery problems that many in North America have only ever seen in textbooks. We worked alongside pediatric neurosurgeon Dr. Emmanuel Wegoye - a Ugandan-born neurosurgeon (and wonderful father, husband, human being!) whose path has taken him to train with awesome pediatric neurosurgeons including Dr. Ben Warf in Uganda and Dr. Graham Fieggen in South Africa. I know this marks the start of years of friendship and collaboration. Healthcare reform is a crucial issue.
While much debate surrounds government finances, I am most concerned about our children's health. Click here to read my blog post in #NeurosurgeryBlog, a forum for health policy. On Dec. 14, 2016 the U.S. Food and Drug Administration (FDA) issued a safety announcement regarding the potential effect of anesthetics on children younger than 3 years of age. The FDA announcement specific points to multiple repeated anesthetics and/or prolonged anesthesia over 3 hours.
Some recent studies suggest that a single, short exposure to general anesthetic and sedation drugs in infants or toddlers is unlikely to have negative effects on behavior or learning. However, much more research is needed to fully understand how early life anesthetic exposure affects children’s brain development. Surgery is scary enough: how should moms and dads evaluate the risk of anesthesia drugs and the possible effects on their baby? Studies are currently ongoing, aiming at characterizing how exposure to anesthesia drugs at a young age may affect children in the long run. The medical and scientific community does not have enough information to be able to draw definitive conclusions at this point. Open, honest conversations are recommended. Families and children's doctors should discuss these issues in the context of each child's care. If a surgery or procedure requiring anesthesia is definitely needed for the health of the child, it should not be delayed. However, if a procedure does not need to be done at an early age, it makes sense to consider the timing. These conversations should be addressed on an individual basis, and families should engage with their physicians to make sure they understand and feel comfortable with choices for their children. Remember, there are no "silly" or "minor" questions with the doctor... it is important for parents to understand and to feel comfortable with choices they are making together with their children's physicians: the choice is for the child and for the family. Here are more resources about this issue:
Being thankful is, in my mind, a way of life. Life is too short and precious for negativity. I was delighted to find this Washington Post article, which provides affirmation on the practice of gratitude. People who practice daily gratitude tend to be happier and healthier.
In this article, reporter Colby Itkowitz interviews researcher Robert Emmons, who studies gratitude. I love the comments. They capture the essence of an approach to life that has gotten me through a lot of good times and tough times. "Gratitude is too good to be left at the Thanksgiving table. I believe that gratitude is the best approach to life. When life is going well, it allows us to celebrate and magnify the goodness. When life is going badly, it provides a perspective by which we can view life in its entirety and not be overwhelmed by temporary circumstances. People who live under an “aura of pervasive thankfulness” reap the rewards of grateful living; conversely, those who fail to feel gratitude cheat themselves out of their experience of life. And why would we want to cheat ourselves? This approach that needs to be cultivated, it’s not going to come easily or automatically. This is when gratitude displays its power and potential. This is when we need to press into our sources of gratitude more deeply — family, faith, freedom — all those circumstances, people, opportunities that we give thanks for each and every day, not just on the fourth Thursday of November." Futher, Emmons comments on dealing with stress and negativity: "Indeed, gratitude rescues us from negativity. Left to their own devices, our minds tend to hijack each and every opportunity for happiness. Negativity, entitlement, resentfulness, forgetfulness, ungratefulness all clamor for our attention. Whether stemming from our own internal thoughts or to the daily news headlines, we are exposed to a constant drip of negativity. Doom and gloom is on the horizon, as financial fears, relational turmoil and health challenges threaten us. Weighed down by negativity, we are worn down, worn out, emotionally and physically exhausted.... We need to constantly and regularly create and take in positive experiences. Gratitude is our best weapon, an ally to counter these internal and external threats that rob us of sustainable joy. In gratitude, we focus on the giftedness of life. We affirm that goodness exists, even among the rancor of daily life. This realization itself is freeing, liberating, redeeming. Gratitude works!" What are you thankful for? Make a list every day. Practice gratitude. Your mind, your health, your friends, your family, your future self will thank you for it. I am thankful for the trust and the faith from my patients and their families. One of my patient's mothers shared her inspiring story in Woman's World magazine, on the newsstands Thanksgiving week. This amazing family reminds us to count our blessings, as they do every day. After epilepsy surgery, little Noah has been seizure-free for over 2 years and counting. It is wonderful to see him grow up and to celebrate his #brainiversary! Read Noah, Mallory, and Craig's story here.
We recently met with Erica Mossholder, the Executive Director of the Children's Craniofacial Association. Check out the CCA website and the terrific work our non-profit partner is doing to empower children and families of kids with craniofacial differences. The #ChooseKind movement is an anti-bullying campaign inspired by the book Wonder by R.J. Palacio. It is a powerful story and life lesson for children and adults alike. The book has opened the conversation about craniofacial differences in classrooms, families, and communities.
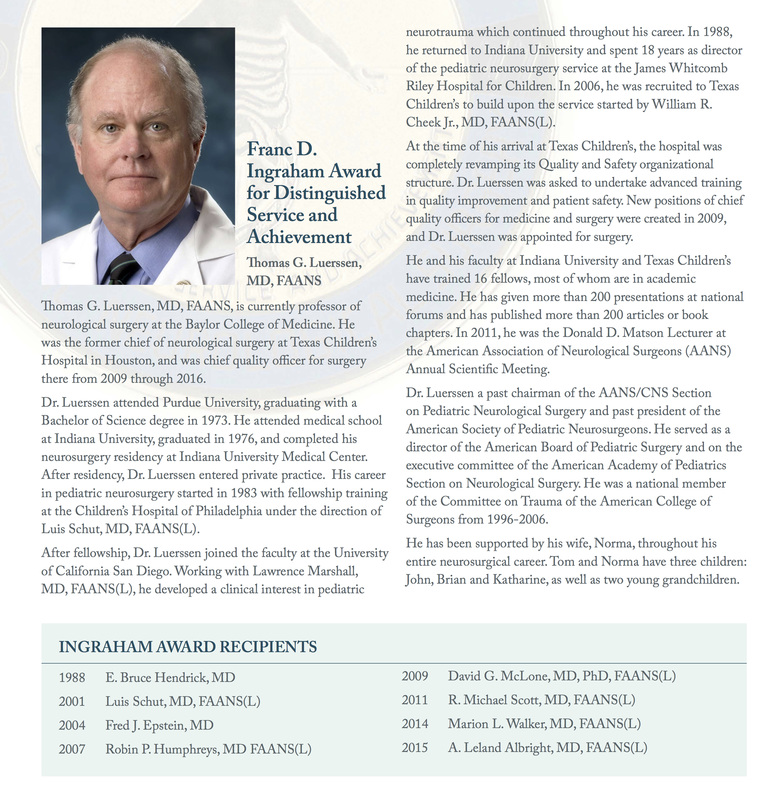
About Wonder by R.J. Palacio from Random House Kids: "August Pullman was born with a facial deformity that, up until now, has prevented him from going to a mainstream school. Starting 5th grade at Beecher Prep, he wants nothing more than to be treated as an ordinary kid—but his new classmates can't get past Auggie's extraordinary face. WONDER by R.J. Palacio begins from Auggie's point of view, but soon switches to include his classmates, his sister, her boyfriend, and others. These perspectives converge in a portrait of one community's struggle with empathy, compassion, and acceptance. In a world where bullying among young people is an epidemic, this is a refreshing new narrative full of heart and hope. R.J. Palacio has called her debut novel "a meditation on kindness"—indeed, every reader will come away with a greater appreciation for the simple courage of friendship. Auggie is a hero to root for, a diamond in the rough who proves that you can't blend in when you were born to stand out." Join the conversation on Twitter: #thewonderofwonder and #ChooseKind Consider the #ChooseKind movement and take the #ChooseKind pledge here. A lifetime achievement award in Pediatric Neurosurgery is only bestowed to a GREAT: someone who has moved the field forward in countless ways and essentially changed the face of Pediatric Neurosurgery. There have only 8 Franc D. Ingraham Award for Distinguished Service and Achievement recipients in history: giants in our field. The last one was my mentor, A. Leland Albright, an incredible person.
The next recipient selected for this honor is my boss and Chief Quality Officer for Surgery at Texas Children's Hospital: Thomas G. Luerssen. The presentation will take place at the AANS/CNS Joint Section on Pediatric Neurosurgery annual conference in Orlando in December 2016. What a special honor to a truly venerable neurosurgeon, colleague, friend, and leader. Our group will be at the conference presenting our scientific research, but more importantly, we will be there to honor the GREAT Dr. Luerssen and his wife Norma who has supported him all the way. Everyone has stories about Tom leading by example, dispensing sage advice, being there no matter what. Some people always know the right way forward: that is Tom. We are so proud he is receiving this highest recognition. When it comes to health and illness, it is hard to plan for life as usual when faced with the unexpected. There are so many unknowns. Hopes, dreams, fears, and uncertainties come together. Daily life routines are not possible. It can be overwhelming. I take care of children with neurosurgery needs, so there is really nothing normal for parents and families as we navigate the journey together. Surgery on your child is undeniably, unquestionably A Big Deal, no matter how routine it might be for the surgery team.
Healthcare journeys are personal, private experiences for some. I have seen incredible inner strength, serenity, and grace. I have also seen examples of inspiring humanity and generosity of communities coming together. The kindness of neighbors, friends, family, and people cannot be underestimated. The conversation can be tough to initiate, both for patient families and for those who would like to help. How does one ask for help when their child is undergoing surgery? On the other side, how does one offer compassion and assistance while respecting space and privacy? Too often, "Let me know if I can help" somehow seems hollow. Considerate action speaks louder than words. There is not a “right” or a “wrong” way. Families have shared wonderful stories with me over the years. Perhaps I can help parents and communities start the conversation if I give some examples that have inspired me. Please feel free to share with parents, families, neighbors, community members, support systems of all types!
Creating a calendar and having meals dropped off at the patient’s house can decompress the family, and allow parents to spend more time with their family member who needs attention. Prepared meals for the entire household ensures everyone is cared for.
Other children or elderly members of the household need supervision and attention while parents are focused on the child receiving healthcare. Offers to take care of the other dependents in the family, even for a few hours (taking them on outings, hosting a sleepover, helping with homework), allows parents to focus on the child who needs more attention at the time. Parents also need time for themselves to recharge and recuperate, to be able to stay strong for the rest of the family.
Mowing the lawn, doing the dishes seem manageable in normal weekly routines, but not when so many things are happening and demanding of the parents’ time and attention. Accepting help does not come naturally to everyone. Many parents decline offers for this type of help, but then realize they are so relieved when these tasks are done.
Children who are part of an activity, a group, or a team are often sad that they cannot participate and belong while they are receiving healthcare treatment and during their recovery process. There are many things organizers, coaches, teammates, teachers, and families can do to assure patients that they are indeed still part of the family and will be welcomed back in any capacity. Signed balls, jerseys, paraphernalia from teammates and classmates Cards, and written or video messages Signs of solidarity: t-shirts, wristbands, symbols of support Honorary memberships (unconditional love and acceptance!)
If it comes from the heart, you cannot go wrong. It takes a village to raise a child. Caring for a family in a time of strain takes a village in thoughtful action. Accept other’s altruism, love, and kindness when in need; pay it forward generously when you are able. I am continually awed by the incredible resilience and beauty of humanity, and humbled to be a part of the journey with families. For the moms and dads who have crossed paths with me -- thank you. |
Pediatric Neurosurgery teamThings we are passionate about Archives
May 2023
Other linksmy TCH blog post on - organizing your medical records for doctor's appointments - Craniosynostosis 101 our patients' moms blog about their family's - epilepsy surgery journey - craniosynostosis surgery journey some of our inspiring patient and family stories in the news: - epilepsy surgery - craniofacial surgery - AVM surgery Cross-post & links to my posts on other sitesUpdates on pediatric cerebrovascular disease in #NeurosurgeryBlog
Comments on health policy, pediatric neurosurgery, and the Affordable Care Act in the #NeurosurgeryBlog Sharing on the "ask-the-doctor" series on the Children's Craniofacial Association's blog - helmet FAQs: after endoscopic craniosynostosis surgery - helmet FAQs: positional plagiocephaly Top rated neuroscience blog
|
SITE MAP |
Content is not medical advice. Disclaimer.
|