|
This is an important landmark - and the only the beginning to more advocacy work around the world.
Folate fortification is only in 23% of countries globally in the year 2023. With appropriate levels of folate fortification in the prenatal period, it is estimated that >300,000 births with neural tube defects such as spina bifida and anencephaly can be prevented every year around the world. Neurosurgeons joined together with global surgeons, public health experts, advocates, geneticists, food scientists, and so many more stakeholders such as my colleagues in the GAPSBIF alliance to advocate for successful support of this resolution at WHA76. --- Repost of a terrific message from stakeholder partner, the International Federation for Spina Bifida and Hydrocephalus: It is with great pleasure that we announce that The seventy-sixth World Health Assembly has voted to adopt the resolution “Accelerating efforts for preventing micronutrient deficiencies and their consequences, including spina bifida and other neural tube defects, through safe and effective food fortification”. This is a tremendous achievement for the global SBH community. This WHO resolution is unique as it combines policies to approach a serious public health crisis with a holistic approach. Combining perspectives from the fields of disability rights, health care and nutrition. Tapping on a global momentum to make a real impact on public health. Read the IF Press Release here. IF, together with partners, and most importantly with IF Members worked together to make this important resolution a reality. In this moment of celebration IF would like to thank you for your extraordinary effort, passion and dedication to the advocacy for this resolution. IF members have been instrumental in reaching national policy makers in effort to get their national governments to support the initiative. The campaign for the WHA Resolution has raised awareness of the importance of cross-sectoral collaborations for public health policies advocacy. To recognise the vital role that each stakeholder has in furthering not only knowledge and awareness but most importantly, achieving policy action. A core principle of disability rights is ‘nothing about us, without us’ and this principle is enshrined in the UN Convention on the Rights of Persons with Disabilities (UNCRPD). During the course of the advocacy for a WHA resolution on large scale food fortification of staple foods with folic acid, the involvement of persons with lived experiences through their representative organisations proved to be an advantage and not just an obligation. The adoption of the WHA Resolution is a moment for celebration. But it is also just the beginning. Moving forward, continued advocacy will be essential in order to ensure effective implementation of the resolution. It is vital that IF and you as Member Associations continue to be involved in the decision making processes regarding policies to reduce the prevalence of spina bifida and other neural tube defects to ensure that these policies are implemented in ways that effectively reach all sections of society and without stigmatising the global SBH community. For increased awareness of the resolution and to begin the campaign for its implementation, IF will continue its advocacy during and after the WHA. Register here.
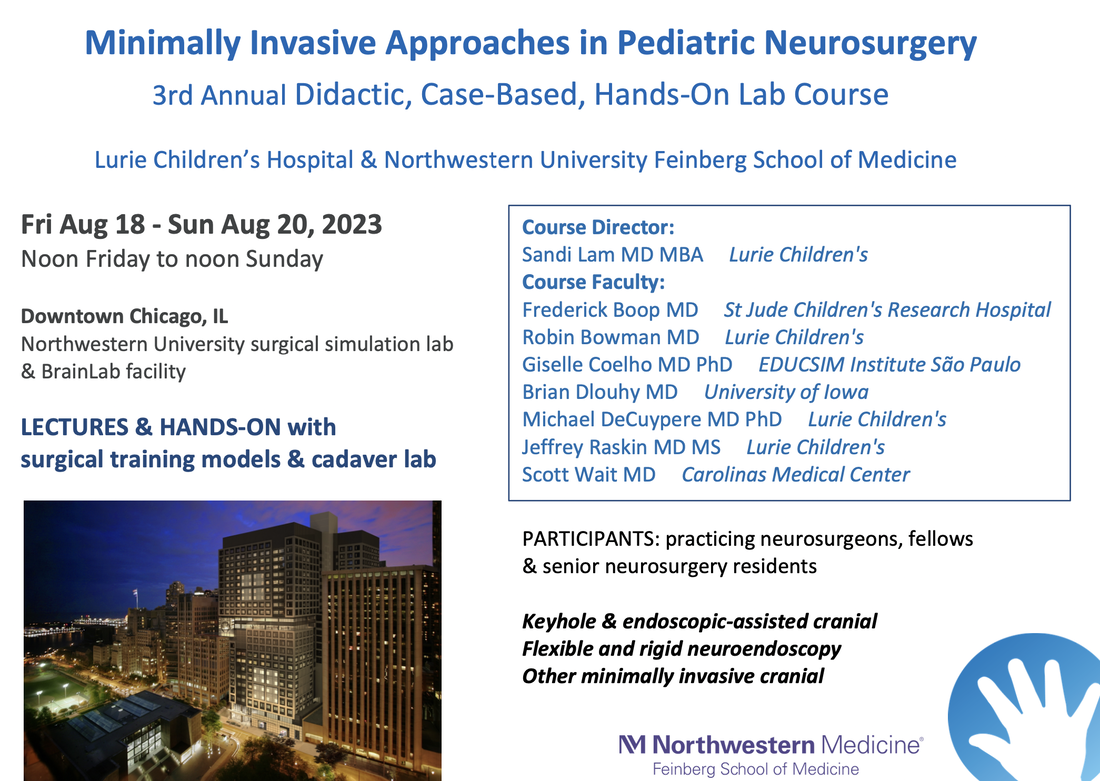
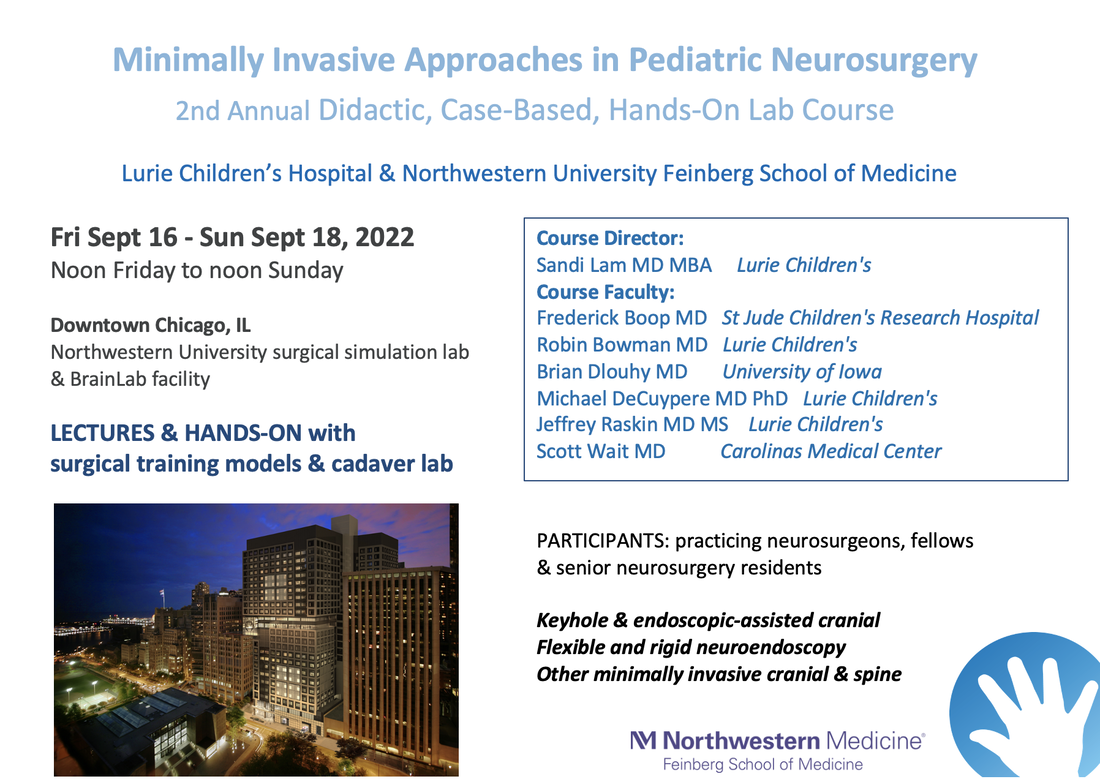
Hotel accommodation included with registration. Official course website and updates on course information here. Inquiries: [email protected] I am thrilled to host this event again. There is no other platform for learning and discussing minimally invasive surgical approaches in pediatric neurosurgery. Here, we have a group of pediatric neurosurgeons who love operating. All have had advanced training in minimally invasive neurosurgery, and have gone on to push the frontiers of the field to achieve better and better outcomes for patients.
For instance, we cover: eyebrow craniotomies and other keyhole approaches in children flexible and rigid neuroendoscopy for tumor, cysts, and hydrocephalus neuroendoscopic lavage endoscopic tumor and epilepsy surgeries fetoscopic techniques minimally invasive spine and functional & more! Register here: https://www.luriechildrens.org/en/events/minimally-invasive-approaches-in-pediatric-neurosurgery--a-didactic-case-based-and-hands-on-course/ We have a great faculty group. Participants last year from the US, South America, and Europe gave rave reviews of the interactive format with a mixture of didactics, case discussions, and hands-on anatomy labs. Two participants even met their future employer and senior partners at the course. This is an exciting annual event that will be a wonderful venue for pediatric neurosurgery & neurosurgery for years to come! In a follow-up to our ongoing initiative with CURE Uganda to develop and elevate pediatric epilepsy care, we congratulate our first global cohort of 10 doctors who completed ASET/Lurie Children's EEG curriculum! We are now engaging in epilepsy conference for case selection for pediatric epilepsy surgery.
It is remarkable how COVID has normalized the use of virtual online collaboration. In our isolation of social distancing and aborted travel during the pandemic, we were able to connect regularly and develop academic and educations experiences that never existed previously. The meaning and the Joy in Work that our teams derived from such a connection over pediatric epilepsy program development was unanticipated. We would not change a minute of it! Read about our journey at the Lurie Children's blog here. Listen to my journey at the Neurosurgery podcast here. Amazing people come together to do amazing things. I have witnessed this through our Global Epilepsy initiative at Lurie Children's and CURE Uganda. The goal was to elevate the offerings of epilepsy care in the region with knowledge and skill transfer in epilepsy surgery, which can produce a surgical cure for seizures in well-selected patients especially with lesional epilepsy. My decade-long relationship with colleagues in subSaharan Africa has only increased my respect and confidence in the surgical skill and dedication of pediatric neurosurgeons like Dr. Emmanuel Wegoye and Dr. Humphrey Okechi. With their service to babies born with congenital neurological problems, these children are now living longer, and facing quality of life issues in chronic diseases such as epilepsy and spasticity. There are an estimated 1000 pediatric patients in the Mbale area who are taking antiseizure medications, who have never received a diagnostic imaging test nor an electroencephalogram (EEG). Without these, we cannot tell if they may benefit from, or be cured with epilepsy surgery. Where do we start? The Lurie Children's EEG team has a successful, established Neurodiagnostic Trechnology training program, fully meeting ABRET accreditation standards. There is donated EEG equipment at CURE. There are no EEG technicians or pediatric neurologists in that part of Uganda. There are many patients in need.abret.org/index.php With these realities in mind, the Lurie Children's Neurodiagnostic technology training program was redesigned to be 24 weeks long, with the goal of producing EEGs on patients in 6 weeks., then further refining skills and troubleshooting over time. The training material and online education portals were donated by the Global Initiative of the Neurodiagnostic Society (ASET), while the twice-a-week hands-on training (by Zoom!) has been conducted by the Lurie Children's team with 10 medical officers and neurosurgeons in Mbale, Uganda. Read more here. Identifying the lateralize, lesional cases is one of the first practical goals. We engage in multidisciplinary epilepsy case conference online and work toward safe, effective pediatric epilepsy surgery care in Uganda and the region. So proud of this initiative - the world is a small, engaged, wonderful place even in the pandemic. We are grateful for this opportunity help make a difference that will continue to grow in impact into the future. Key facts from the WHO about Epilepsy:
I have had the honor of working in amazing families to learn about their epilepsy journeys and to develop informative on-demand webinars to address frequently asked questions. November is Epilepsy Awareness Month, which provides a spotlight for a journey that we work on every single day of every year. #LetsTalkAboutEpilepsySurgery is a terrific initiative started by Monika Jones JD at the Brain Recovery Project. I was honored to take part and discuss different types of epilepsy surgery for families approaching and considering these options for the first time. This is a great resource with a repository of a series of webinars with surgeons, epileptologists, providers, and advocates for pediatric epilepsy. Neurostimulation is also a surgical option that is offering hope to those who may not have been considered surgical candidates before. My brilliant epilepsy colleague Dr. Joyce Wu and I joined Shae's mom along with Gabrielle Conecker and JayEtta Hecker of DEE-P Connections for a deep dive discussion in this webinar about Stimulators: Could a VNS, DBS, or RNS help?
I am grateful for the privilege of working with children and their amazing families. They inspire me every day. It is incredible that my minimally invasive endoscopic epilepsy surgery program has been able to help many young children and young adults. Baby Aurora's family shares their uplifting story and experience with endoscopic hemispherotomy. They traveled across country borders and state lines, and they felt that they were in the right place. The feeling is mutual. Ready about them in "Pediatric Neurosurgeon Halts Baby's Seizures with Minimally Invasive Brain Surgery."
Never before has there been such fertile ground in developing Health Services Research, Global Health, and Quality & Safety in Pediatric Neurosurgery. Currently, we are accepting applications for funded positions for neurosurgery residents in North America to spend 1-2 years with our team to do specialized health services, global health, and/or quality/safety research in pediatric neurosurgery as Research Scholars.
Whether it is working with one of the longest running and most active multidisciplinary spina bifida programs in the country, the Chicago Center for Fetal Medicine, the Healthy Communities initiative, Northwestern's Institute for Public Health and Medicine, Northwestern's Institute for Global Health, Center for Education in Health Studies, the Smith Child Health Research, Outreach, and Advocacy Center, and the highly ranked Northwestern Department of Neurosurgery, collaborative opportunities abound for research scholars and trainees joining our team. We understand that health is more than healthcare. As Lurie Children's mission is to improve the health and well-being in children, we in Pediatric Neurosurgery believe in expanding our sights beyond perfecting neurosurgical technique and beyond discoveries in the basic science labs. Building bridges across all pillars of pediatric research will translate discoveries from bench to bedside, to the population and into policy to help all children. For instance, we want to know why patients have difficulties getting to neurosurgical attention, when we know we have surgical solutions to offer for diseases like epilepsy. At Lurie Children's, leaders like Dr. Matt Davis, chairman of pediatrics, leads funded community initiatives to work within and outside the walls of the hospital in partnership with community leaders and organizations, knowing that life expectancy at birth can vary by 17 years depending on the neighborhood in Chicago. We will partner with such initiatives to expand the reach of neurosurgery, so that we can characterize and understand disparities, barriers in access to care, and predictors of outcomes that go beyond surgical technique; taking it a step further, the community and state partnerships will allow a forum for intervention and building models for effective, inclusive care. That is one example above; other projects as well as global health opportunities are also in the works. We invite neurosurgery residents in North America to spend 1-2 years with our team to do specialized health services, global health, and/or quality/safety research in pediatric neurosurgery as funded Research Scholars. This pediatric-neurosurgery-specific forum is the first of its kind. We also have visiting research and observership positions for international colleagues to learn about pediatric neurosurgery at Lurie Children's as we work on studying neurosurgical healthcare delivery both locally, nationally, and globally. Our funded initiatives in epilepsy and spina bifida will be a start, and we will develop within this rich, socially-responsible, active research community to work toward the promise of a cure, the promise of safer space, and the promise of a healthier future. Learn more and apply by contacting [email protected] I am grateful to have the opportunity to work with neurosurgery colleagues around the world. This summer, I was invited to travel to Taipei to help in a case of a child with rapid decline and worsening intractable epilepsy. A multi-institutional and multidisciplinary epilepsy surgery conference was held, and the consensus was to offer hemispherectomy surgery. I operated with her local neurosurgeons, applying the minimally invasive endoscopic hemispherotomy technique I have published. This week, the girl and her family held a press conference with her team at the National Taiwan University Children's Hospital. I was able to teleconference in: she waved brightly and said thank you to me. That is the most wonderful Thanksgiving message I can remember.
Story in Chinese here. Thank you to the team at Lurie Children's for their support! Endoscopic hemispherotomy featured as one of the top innovations from Texas Medical Center7/28/2019
Houstonia Magazine highlighted top 5 breakthrough developments in the Texas Medical Center this year: it is an honor to report that my work in endoscopic hemispherotomy surgery for epilepsy is one of them.
Click here to see the feature by Morgan Kinney in the August 2019 issue of Houstonia. |
Pediatric Neurosurgery teamThings we are passionate about Archives
May 2023
Other linksmy TCH blog post on - organizing your medical records for doctor's appointments - Craniosynostosis 101 our patients' moms blog about their family's - epilepsy surgery journey - craniosynostosis surgery journey some of our inspiring patient and family stories in the news: - epilepsy surgery - craniofacial surgery - AVM surgery Cross-post & links to my posts on other sitesUpdates on pediatric cerebrovascular disease in #NeurosurgeryBlog
Comments on health policy, pediatric neurosurgery, and the Affordable Care Act in the #NeurosurgeryBlog Sharing on the "ask-the-doctor" series on the Children's Craniofacial Association's blog - helmet FAQs: after endoscopic craniosynostosis surgery - helmet FAQs: positional plagiocephaly Top rated neuroscience blog
|
SITE MAP |
Content is not medical advice. Disclaimer.
|